Introduction
Cognitive Behavioral Therapy (CBT) is a widely recognized, evidence-based form of psychotherapy designed to address and transform negative thought patterns, improve emotional regulation, and foster constructive behavioral changes. CBT has proven effective in treating a range of psychological conditions such as depression, anxiety, PTSD, addiction, and more, offering individuals a structured path to improved mental well-being.
Table of Contents
Cognitive Behavioral Therapy (CBT)
History and Development of CBT
CBT’s roots can be traced back to the 1960s, combining elements of behavior therapy (from figures like B.F. Skinner and Ivan Pavlov) with cognitive therapy pioneered by Aaron Beck. Beck’s work highlighted how distorted thinking patterns fuel emotional disturbances, laying the foundation for modern CBT, which combines cognitive and behavioral approaches to address both thought patterns and actions.
Principles of Cognitive Behavioral Therapy
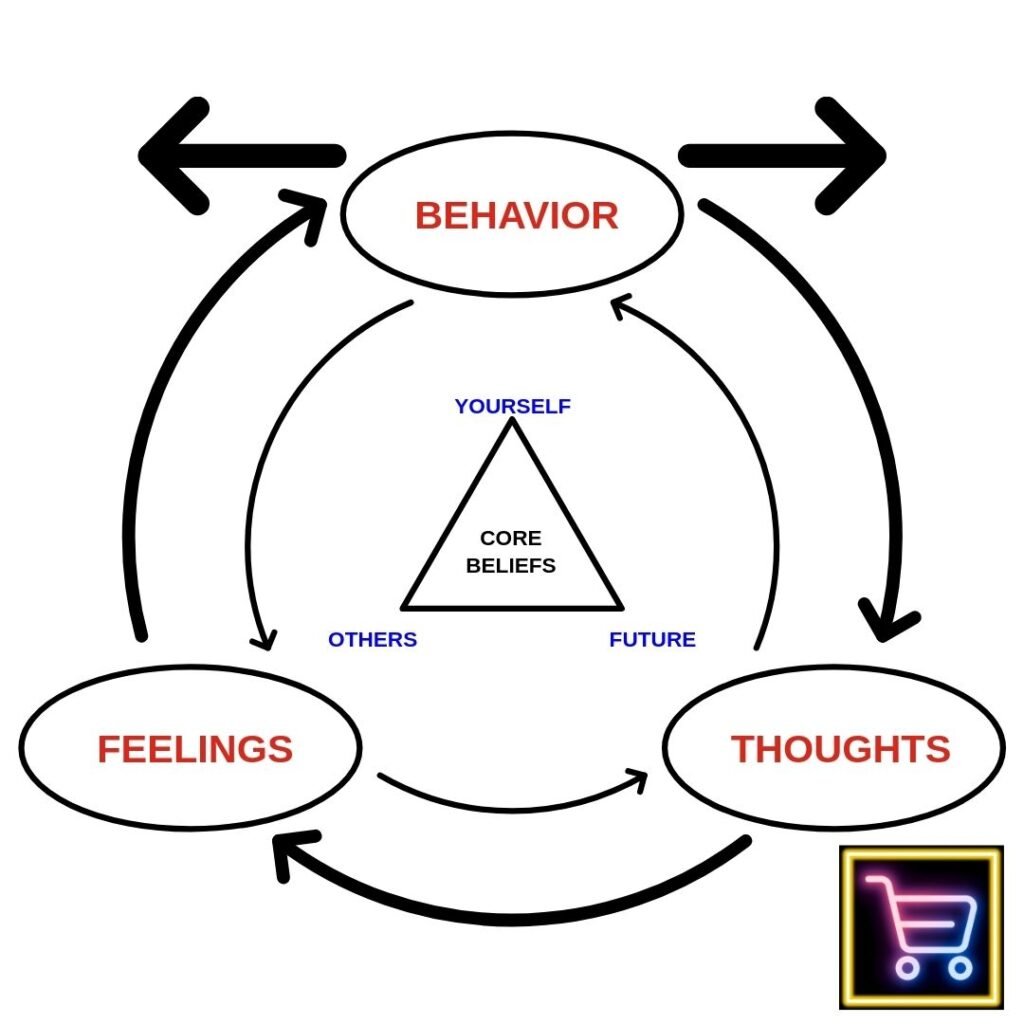
1. Thought Patterns and Cognitive Distortions
- Automatic Negative Thoughts (ANTs): These are habitual, often unconscious, thoughts that can lead to self-defeating behavior.
- Cognitive Distortions: Common distortions include catastrophizing, overgeneralization, and black-and-white thinking, which CBT seeks to identify and correct.
2. Behavioral Changes
- Behavior plays a significant role in reinforcing thoughts and emotions. CBT uses behavioral experiments and exposure therapy to challenge harmful behaviors and cultivate positive alternatives.
3. Goal-Oriented and Solution-Focused
- CBT is typically short-term, focusing on specific goals and measurable outcomes, which makes it a structured and practical approach to therapy.
Cognitive Behavioral Therapy: Techniques and Approaches
CBT employs a range of techniques, often tailored to each individual’s needs and goals. Commonly used techniques include:
| CBT Technique | Description |
|---|---|
| Cognitive Restructuring | Identifying and reframing negative thoughts, allowing for a more balanced perspective. |
| Behavioral Activation | Increasing engagement in enjoyable or meaningful activities to improve mood and motivation. |
| Exposure Therapy | Gradual exposure to feared situations or stimuli to reduce anxiety or phobia over time. |
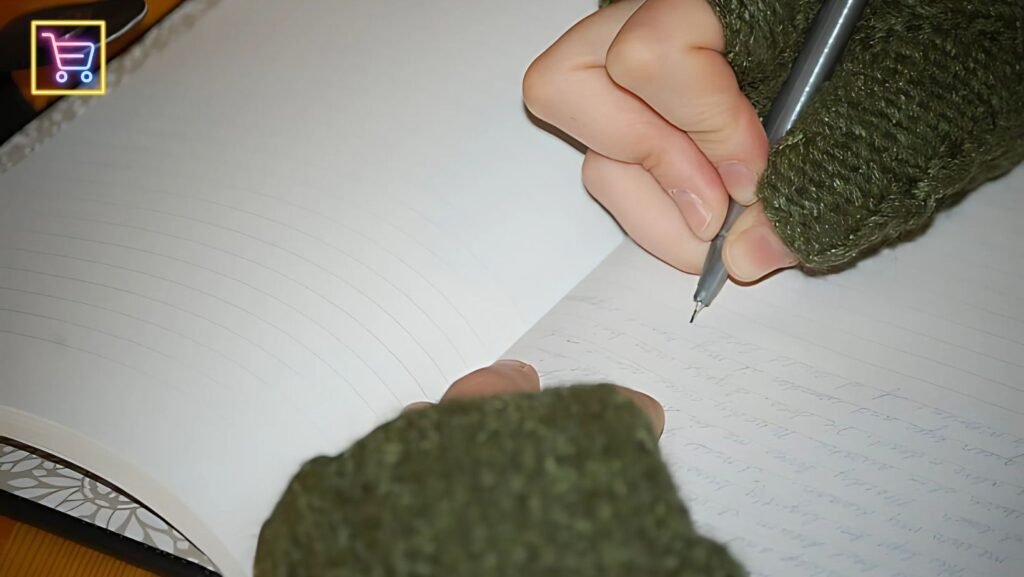
| Journaling | Writing about experiences, emotions, and triggers to better understand personal thought patterns. |
| Mindfulness Techniques | Fostering present-moment awareness to better observe thoughts and feelings without judgment. |
| Progressive Muscle Relaxation | Using physical relaxation exercises to reduce tension and improve emotional regulation. |
How Does CBT Work?
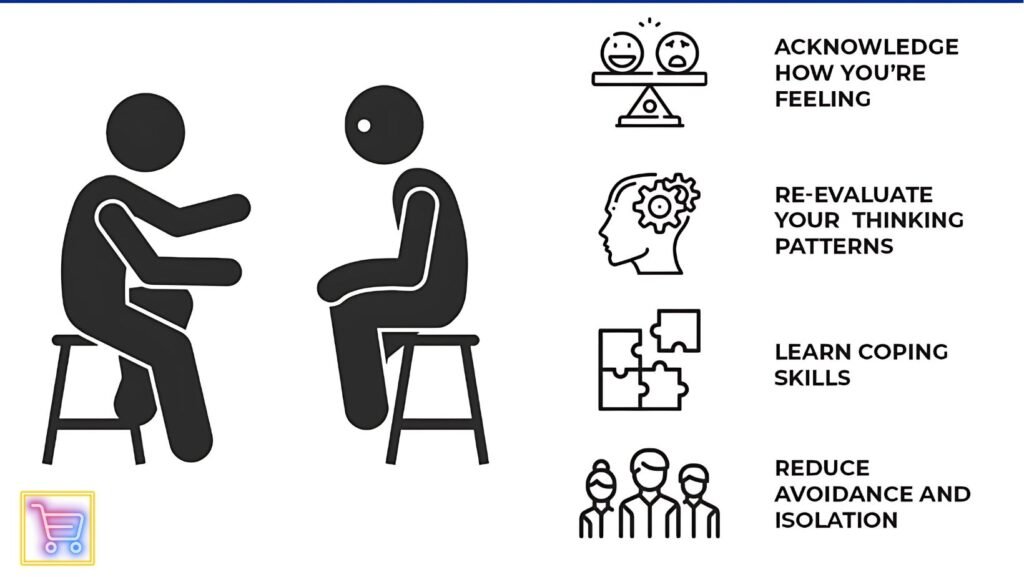
CBT emphasizes a collaborative, active engagement between therapist and patient. Therapy typically follows a structured, step-by-step process involving:
- Assessment: Identifying problematic thoughts and behaviors.
- Goal Setting: Creating specific, measurable, and achievable objectives.
- Skill Development: Learning and practicing CBT techniques, such as cognitive restructuring and mindfulness.
- Practice and Homework: Between-session assignments that reinforce skills.
- Evaluation and Adjustment: Continuously assessing progress and adjusting techniques as necessary.
Benefits of Cognitive Behavioral Therapy
CBT’s structured, goal-oriented nature contributes to its effectiveness. Here are some documented benefits:
- Effectiveness Across Conditions: Studies show CBT has a high success rate in treating conditions like depression, anxiety, and PTSD.
- Long-Term Results: CBT equips individuals with tools to manage future challenges, resulting in sustained benefits.
- Limited Side Effects: Compared to pharmacological treatments, CBT is non-invasive with minimal side effects.
Table: Conditions Commonly Treated with CBT
| Condition | CBT Success Rate (%) | Common Techniques Used |
|---|---|---|
| Depression | 50-75% | Cognitive restructuring, behavioral activation |
| Generalized Anxiety Disorder | 60-75% | Exposure therapy, journaling, cognitive restructuring |
| Post-Traumatic Stress Disorder (PTSD) | 60-80% | Exposure therapy, mindfulness |
| Obsessive-Compulsive Disorder (OCD) | 60-70% | Exposure and response prevention |
Source: American Psychological Association, 2023
CBT for Specific Populations
- Children and Adolescents: CBT is increasingly used to help young people with behavioral and emotional challenges, especially as it can be adapted to suit developmental needs.
- Older Adults: With modifications, CBT can help older adults cope with age-related concerns like grief, loneliness, and cognitive decline.
- Individuals with Chronic Illness: CBT can be effective in managing the emotional impact of chronic illness, helping individuals adopt coping strategies to enhance their quality of life.
Statistics on CBT’s Effectiveness
CBT’s reputation is backed by extensive research showing high success rates in mental health treatment. According to a study published in JAMA Psychiatry:
- 60% of individuals with generalized anxiety disorder reported improved symptoms after 12 sessions of CBT.
- 55-60% of those with depression saw significant improvement following 16-20 sessions.
- 75% of individuals with posttraumatic stress disorder benefited from exposure therapy techniques within CBT.
Source: JAMA Psychiatry, 2022
Challenges and Criticisms of CBT
Although highly effective, CBT is not without its limitations. Some criticisms include:
- Doesn’t Address Deep-Rooted Issues: Critics argue that CBT’s focus on immediate thoughts and behaviors can overlook underlying psychological causes.
- Requires Patient Commitment: For CBT to be effective, patients must actively engage with assignments outside of sessions, which can be a barrier for some.
- May not suit all individuals: CBT may be less effective for those with complex mental health needs, where a more integrative approach may be preferable.
Comparison of CBT with Other Therapies
| Therapy Type | Focus | Duration | Best Suited For |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Thought patterns and behaviors | Short-term (8-20 weeks) | Depression, anxiety, PTSD, phobias |
| Dialectical Behavior Therapy (DBT) | Emotional regulation | Long-term | Borderline Personality Disorder, self-harm behaviors |
| Psychodynamic Therapy | Exploring unconscious influences | Long-term | Chronic mental health issues, complex trauma |
| Interpersonal Therapy (IPT) | Social and relationship skills | Short-term | Depression, social anxiety, relational issues |
How to Begin CBT: Finding the Right Therapist

When searching for a therapist trained in CBT:
- Certification and Training: Look for therapists who are certified by credible organizations like the Academy of Cognitive Therapy.
- Experience with Your Condition: Choose a therapist with experience treating your specific issue.
- Comfort Level: The therapeutic relationship is essential to success, so select someone with whom you feel comfortable.
DIY Cognitive Behavioral Techniques for Self-Help
While a trained therapist can guide you through CBT, there are self-help techniques that may help you begin to manage negative thought patterns and behaviors:
- Thought Records: Track negative thoughts and analyze their accuracy.
- Behavioral Experiments: Challenge your fears by testing whether your thoughts hold true.
- Gratitude Journaling: Foster positive emotions by recording what you’re grateful for.
Conclusion: Why Cognitive Behavioral Therapy Is a Leading Choice for Mental Health Care
CBT’s evidence-based approach, focus on skill-building, and adaptability to various mental health conditions make it an effective choice for many. As one of the most widely researched psychotherapies, CBT’s structured and collaborative framework offers individuals practical tools to manage their mental health effectively.
References
- American Psychological Association. (2023). Clinical Practice Guidelines for the Treatment of Depression and Anxiety.
- Beck, A. T. (1967). Depression: clinical, experimental, and theoretical aspects. Harper & Row.
- Journal of the American Medical Association Psychiatry. (2022). The Effectiveness of Cognitive Behavioral Therapy for Various Disorders.